IAHSS Foundation
The International Association for Healthcare Security and Safety (IAHSS) Foundation was established to foster and promote the welfare of the public through education and research and the development of a healthcare security and safety body of knowledge. The IAHSS Foundation promotes and develops research to further the maintenance and improvement of healthcare security and safety management, and it develops and conducts educational programs for the public. For more information, please visit www.iahssf.org. The IAHSS Foundation is completely dependent on the charitable donations of individuals, corporations and organizations. Please help us continue our mission and our support of the healthcare industry and the security and safety professionals who serve institutions, staff and, most importantly, patients. To donate or to learn more about the IAHSS Foundation, please visit the website or contact Nancy Felesena at (888) 353- 0990.
Thank you for your continued support.
Ronald Hawkins
Research Committee Chair
IAHSS Foundation
IAHSS Foundation Board of Directors
Bill Navejar
President
Ashley Ditta, CHPA
Treasurer
Bonnie Michelman, CHPA, CPP
Massachusetts General Hospital
Steve Nibbelink, CHPA, CA-AM
Secure Care Products
Brigid Roberson, Ed.D., CHPA
Texas Medical Center
Chad Rioux, CHPA, CPP
Motorola Solutions
Paul Greenwood, CHPA
Unity Health Toronto
Scott Hill, Ed.D., CHPA, CPP
King’s Daughters Health System
Marilyn Hollier, CHPA, CPP
Security Risk Management Consultants
Ronald Hawkins
Security Industry Association
Roy Williams III, CHPA
Download PDF copy of the document
INTRODUCTION
Homelessness is a concern for many people in the United States and around the world. Though estimates vary around the world, as of 2018, over 550,000 individuals experienced homelessness every day (Henry et al., 2018). However, methodologies to measure homelessness vary even in the United States and may underestimate the number of homeless members in the population (Schneider et al., 2016). Descriptive data is often challenging to acquire for the homeless population as there usually is not a specific sampling frame for national surveys to ensure people who are homeless are included in national statistics (Patten, 2017).
The homeless populations in the United States and abroad pose concern for hospitals to understand how to best provide care and support. People who are homeless often have mental health and general health issues that should be considered when providing treatment (Hwang & Burns, 2014). Life expectancy for this group is estimated to be up to of 30 years lower than non-homeless patients (Davies & Wood, 2018). With the move away from homelessness a criminal issue and towards a health problem, more burden for care has come on health care workers to provide support (Hanssmann et al., 2022).
The purpose of this review is to understand how healthcare workers can facilitate a safe and quality environment for homeless patients both in the hospital and upon discharge. By identifying specific challenges and concerns with the homeless populations and both national and international interventions and policies that have previously been established that may help foster an environment that is supportive of the homeless patients.
REVIEW OF LITERATURE
There are many concerns related to the homeless population both within the community and hospital settings. These include many general health, mental health, and safety concerns that need to be addressed at multiple levels.
General Health Concerns
Understanding the health concerns of the homeless population can be challenging. Patients that were homeless and providers in an emergency department in Australia were interviewed on the health-related areas they felt were important (Moore et al., 2011). The results of the interview identified many complex issues such as a lack of familial and social support, mental health and substance abuse issues, the absence of respect for the patient or development of relationship by the providers, no after-hours options other than the emergency room, and not having the resources required to treat the patients (Moore et al., 2011). The varying degrees of responses in the study highlighted the challenges associated with homelessness and the difficulties in accessing the necessary healthcare in a timely manner (Moore et al., 2011).
When the Boston, Massachusetts Medicaid population was evaluated, people who were homeless were more likely to use emergency department resources rather than other healthcare services when compared to those who were not homeless (Lin et al., 2015). Additionally, hospitalizations were higher among the homeless group compared to the group who was housed (Lin et al., 2015). Since the homeless are more likely to use emergency rooms compared to those who are not, a hospital closing can have a more detrimental effect on homeless patients (Gummerson et al., 2022). A closing hospital may require homeless patients to travel further to receive care and also increases the number of resources and staff required for neighboring hospitals to keep up with the intensified demand in the emergency department (Gummerson et al., 2022).
Another common occurrence is for people who are homeless to visit the emergency room since they do not have food, shelter, or other basic needs covered at the time of their visit (Rodriguez et al., 2009). Patients in the emergency department who were homeless were also more likely to have at least one social deprivation, such as no food, heat, electricity, or were evicted (Gordon et al., 2001). One study found over 70% of homeless patients visited the emergency room for an “inappropriate” reason, meaning they were not presenting with true clinical needs at the time of their visit (Han & Wells, 2003). “Frequent flyers” in hospitals refer to patients who often visit the emergency department unnecessarily and are a burden to hospital resources (Fulde & Duffy, 2006; Malone, 1998; Ruger et al., 2004). Homeless patients have been considered frequent flyers when they utilize the emergency room to avoid the unsafe and inconvenient alternatives they have (Malone, 1998).
Differences in adequate diagnosis and treatment at hospitals were present among homeless and non-homeless patients presenting with acute myocardial infarction or stroke in four states in 2014 (Miyawaki et al., 2021). Patients that were homeless and presenting with an acute myocardial infarction were less likely to have a coronary angiogram as well as percutaneous coronary intervention or coronary artery bypass grafting surgery for treatment compared to patients who were not homeless in a traditional hospital setting (Miyawaki et al., 2021). However, these significant differences in diagnosis and treatment were not observed in the safety-net hospital setting, though all patients regardless of housing status were more likely to have inadequate diagnosis and treatment procedures than in a traditional hospital (Miyawaki et al., 2021). For stroke patients, homeless patients had lower odds of receiving a cerebral arteriography compared to non-homeless patients (Miyawaki et al., 2021). In the safety-net hospitals, no differences in treatments for stroke patients between those who were homeless and those who were not observed (Miyawaki et al., 2021). Nonetheless, these differences observed between the homeless and non-homeless patients in safety-net and traditional hospitals were not associated with an increase in death for either stroke or myocardial infarction patients (Miyawaki et al., 2021). This contrasts with another study conducted in 3 states to measure the mortality rate of cardiovascular conditions in general over a span of almost 5 years (Wadhera et al., 2020). While this study found similar differences in treatment between the homeless and non-homeless patients that were hospitalized, mortality rates for stroke and cardiac arrest were significantly higher among those who were homeless compared to those who were not, though did not differ for heart failure (Wadhera et al., 2020).
Breast cancer patients who were homeless had a delayed treatment of more than 30 days after diagnosis compared to patients who were not homeless (Festa et al., 2020). Since successful cancer treatment relies on early diagnosis and treatment, any delay in treatment can alter the prognosis of the disease in the patients (Festa et al., 2020). The most documented reason for the delay in treatment was mental illnesses, comorbid conditions, changes in housing situation, financial concerns, and no location for post-surgery recovery (Festa et al., 2020). A recent meta-analysis found that people experiencing homelessness reported an average of .72 to 5.8 visits to the emergency department in a year (Vohra et al., 2022). The most common reason for the visits was alcohol-related incidents and general injuries (Vohra et al., 2022). Differences in health characteristics and uses of the healthcare systems may vary based on whether people are newly homeless, episodically homeless, or chronically homeless (Cox et al., 2017). Furthermore, almost 30% of homeless patients with Medicaid in Boston were readmitted within 30 days of a visit (Racine et al., 2020). End-of-life care for the homeless population is a challenging area since it often requires the coordination of many different organizations and providers (van Dongen et al., 2020). Gaps in care may further complicate end-of-life care especially if safety issues arise in the hospital/treatment setting like smoking while on oxygen or providing illicit drugs for other patients which forces a homeless patient to leave this setting when treatment is needed most (van Dongen et al., 2020). It is often difficult to determine which types of end-of-life treatments and care plans may be required for the homeless population, however, about three-fourths of homeless patients had to be removed from the shelter before end-of-life (van Dongen et al., 2020). Community-based participatory research in Connecticut identified some barriers associated with homeless patients that included the following: under-recognition of homelessness in the hospital leading to not obtaining resources available; provider attitudes negatively impact care; the need for improved follow-up and discharge plans; and medical needs are hard to manage/prioritize when other basic needs are unmet (Franco et al., 2021). Similarly, the homeless population in Brazil identified many barriers to maintaining health and accessing healthcare (Prado et al., 2021). This population also identified an issue of the lack of follow-up from healthcare workers after leaving healthcare services in addition to having to be more “aggressive” towards healthcare workers to get the help they require (Prado et al., 2021). A systematic review of studies around the world identified several major and sub-themes including lack of basic physical, social, and resources needed to access care; feelings of discrimination and negative stigmatism and the need for supportive relationships; and other barriers that were structural or organizational that failed to meet the multifaceted needs the homeless population face (Omerov et al., 2020).
Mental Health Concerns
One major concern among the homeless population is the rampant mental health conditions. An international pool of estimates of homeless populations in many western countries found many individuals were experiencing at least one form of mental illness (Fazel et al., 2008). The pooled sample showed the most common illnesses including 37.9% with alcohol dependence and 24.4% with drug dependence (Fazel et al., 2008). Furthermore, 12.7% of the pooled estimate of the homeless population worldwide had a psychotic illness, 11.4% had major depression and 23.1% had a personality disorder (Fazel et al., 2008). A systematic review of the homeless population in Germany estimated that 77.5% had some form of mental illness (Schreiter et al., 2017). Substance abuse and alcohol or drug dependency were the most prevalent (Schreiter et al., 2017). The high prevalence of mental health conditions among the homeless population helps inform community and healthcare workers who may interact with these individuals.
Patients with mental health conditions were more likely to be readmitted within 30 days to the emergency department than those without mental health conditions (Lam et al., 2016). When adjusted for homelessness, the likelihood of readmission to the emergency department and hospitalization within 30 days of an emergency department visit increased significantly (Lam et al., 2016). Homeless persons with alcohol dependence are more likely to be deficient in several key vitamins, which may lead to exacerbated medical problems (Ijaz et al., 2017). More specifically, vitamins C and B1, as well as small deficiencies in vitamin E and other B vitamins (Tornero Patricio et al., 2016).
Safety Concerns
For those who are homeless, shelters are often relied on to provide protection, however, a qualitative research study found that many homeless people reported that the homeless shelters were not safe due to violence, drugs, and theft (Kryda & Compton, 2008). Drug presence is especially dangerous for those who have substance abuse issues (Kryda & Compton, 2008). Additionally, some found jail to be a safer environment than some homeless shelters (Kryda & Compton, 2008).
Patients who were homeless were more likely to have experienced violence in the last two weeks upon arrival to the emergency department compared to those who were not homeless, especially among those who also have a mental illness (Dale E. McNiel & Renée L. Binder, 2005). Violent attacks were more likely among people who were older and homeless for two or more years (Meinbresse et al.). Among homeless patients with Schizophrenia and Bipolar Disorder in France, over one-third reported they were violent either verbally or physically towards another person within the last 6 months (Fond et al., 2019).
A recent meta-analysis evaluated pooled estimates for suicidal attempts among specific characteristics of the homeless population and found that over 30% of homeless people in North America had made a suicide attempt (Xiang et al., 2021). Heterosexual individuals and males were at a lower risk for suicide attempts than non-heterosexual people and females (Xiang et al., 2021). Childhood sexual abuse, trauma, and mental health disorders were all associated with an increased likelihood of a suicide attempt
(Xiang et al., 2021).
A study from a safety-net hospital identified key safety concerns among the patients that were homeless (Jackson et al., 2019). Over 20% slept in the street or another location not intended to be slept in (Jackson et al., 2019). Almost 20% of patients who were homeless at one safety-net hospital reported they had been attacked in the streets
(Jackson et al., 2019). Another study found that in a safety-net setting, homeless patients were significantly more likely to report inadequate communication from hospital staff regarding their medications compared to patients who were not homeless
(Vellozzi-Averhoff et al., 2021).
Opioid usage and overdoes are an issue, especially among veterans who are homeless in the United States (Midboe et al., 2019; Soncrant et al., 2021). Older veterans that were homeless were more likely to receive a risky dose of opioids after an opioid usage disorder overdose without a Naloxone prescription and medicine for addiction treatment (Midboe et al., 2019). Veterans who were homeless were more likely to have an opioid overdosing event and attempt or successfully complete suicide than those who were not homeless (Soncrant et al., 2021). In this population, adverse events were often preceded by a delay in receiving health care as well as discharge confusion (Soncrant et al., 2021). A similar study found that homeless veterans were almost 3 times as likely to die from suicide as those who were not homeless, over 7 times as likely to die from homicide, and more likely to die a year younger than those who were not homeless (Schinka et al., 2018).
A study in Scotland found that the homeless population in Glasgow had a significantly higher incidence of head injuries in the hospital than the overall city incidence (McMillan et al., 2015). Even among those who were not hospitalized for their head injury, the homeless population with a head injury that later died over 30 years was much higher than the general population (McMillan et al., 2015). Similar findings were observed in Pennsylvania, where alcohol-positive traumatic brain injury was higher among homeless patients than non-homeless patients (Dell et al., 2021).
Among homeless patients who died by suicide, 21% died while in in-patient care, which was double the percentage in the non-homeless population (Culatto et al., 2021). The homeless patients that died by suicide were also more likely to have been treated for self-harm in emergency departments prior to suicide as well as enrolled in either drug or alcohol services compared to the non-homeless patients that died by suicide (Culatto et al., 2021). Of the inpatients that were homeless and died by suicide, almost half had left the ward (or failed to return) without permission from hospital staff (Culatto et al., 2021). In the week to 3 months after being released from the hospital, there were higher incidences of suicide among the homeless population than in the non-homeless population (Culatto et al., 2021). Functional impairment as people in the homeless population age is another safety concern that must be addressed (Cimino et al., 2015). Basic needs of everyday life become more challenging to include getting dressed, eating, and transferring from one spot to another (Cox et al., 2017). If left unmonitored, these could have dangerous implications for those who are homeless (Cox et al., 2017).
GUIDANCE FOR POLICIES AND INTERVENTIONS IN U.S. HOSPITALS
Not having a place to sleep inhibits the ability to be as healthy as possible, thus healthcare workers often try to provide opportunities for homeless patients to be eligible to receive housing (Hanssmann et al., 2022). One specific hospital intervention involved a series of achievements patients were to reach before “graduating” and extensive data tracking patients to ensure they are moving through the program (Hanssmann et al., 2022). By providing this intervention, the patients were able to reach biomedical stabilization and thus hopefully require less hospital access in the future (Hanssmann et al., 2022).
To address hospital frequent flyers, a few interventions have been successful. A program in New York City called “Salud a Su Alcance” also known as “Health Care within your Reach,” was an emergency department initiative involving health priority specialists and community health workers to help redirect patients who more frequently visited hospital emergency department to other types of care as deemed appropriate
(Michelen et al., 2006). This hospital and community-based approach resulted in a significant reduction in emergency department visits from previously identified frequent flyers (Michelen et al., 2006). Multidisciplinary case management, including using hospital care and community resources, was also beneficial for reducing frequent flyers in the hospital emergency department (Phillips et al., 2006).
For veterans who were homeless with severe mental illnesses, providing healthcare clinics that were specifically designed for the homeless population improved patient satisfaction and access to care (Gabrielian et al., 2021). Homeless-Patient Aligned Care Teams were established in 2012 to be more accessible to veterans who were homeless, especially among those with severe mental illnesses (Gabrielian et al., 2021). Overall, patients in the Homeless-Patient Aligned Care Teams had better access and coordination, better relationships with their physicians, and coordination and cooperation when compared to homeless veteran patients who did not receive care from the specialized teams (Gabrielian et al., 2021). However, of the care teams’ surveys, less than 30% had at least 3-4 services included in the care setting (such as housing coordination, social work, etc.), which shows areas of improvement for future endeavors (Gabrielian et al., 2021).
Transdiagnostic treatment protocols such as the Unified Protocol may help treat mental and physical comorbidities in the homeless population (Sauer-Zavala et al., 2019). A pilot program of the Unified Protocol in a safety-net hospital showed the protocol was fairly simple for staff to understand and implement (Sauer-Zavala et al., 2019). Patients improved in several skills outlined in the protocol which is promising that the Unified Protocol may be a valuable evidenced-based tool to improve mental health in a variety of contexts (Sauer-Zavala et al., 2019).
“A SAFE DC” program is an acronym that outlines seven components to addressing homeless patient needs in the hospital and upon discharge (Best & Young, 2009). First, assessing the housing situation of patients upon arrival to determine what type of services at discharge and follow-up may be required (Best & Young, 2009). Next, screening and prevention will provide a full medical exam to ensure no undiagnosed conditions exist and educate on specific dangers such as infectious needles with drug usage (Best & Young, 2009). This protocol includes an accelerated Hepatitis B immunization schedule to reduce risks (Best & Young, 2009; Wright et al., 2002).
Addressing primary care issues is the next step and recommends the healthcare worker provide any medication and treatment that may be required that is traditionally handled by a primary care provider like disease screenings, vaccinations, and blood pressure management (Best & Young, 2009). Follow-up care is often more challenging since there may be no primary care provider; thus, providing the patient with a printed copy of the discharge materials and either making any necessary follow-up appointments or a referral to an “aftercare” clinic may be beneficial to improving patient health (Best & Young, 2009). End-of-life discussions should be held so the patients who are homeless know the options available to them and can make their preferences known (Best & Young, 2009). Discharge instructions should be simple and realistic since many patients and their support system may be health illiterate so it is imperative that instructions are thorough and easy to follow to reduce the risk of medication lapse or complications (Best & Young, 2009). The final aspect of the “A SAFE DC” model is communication after discharge should be made known to ensure the healthcare workers can reach the patient with test results or any other follow-up that may need to happen (Best & Young, 2009). The “A SAFE DC” is a thorough framework that healthcare workers may follow to ensure patients that are homeless can be as safe as possible upon discharge. Nurse-led interventions have also been valuable in improving the health and safety of homeless patients (Weber, 2019). Nurses working as the primary contact and/or care managers helped increase medication adherence and improve mental health and quality of care (Weber, 2019). Other nurse interventions involved the nurse delivering group therapy or education materials that offered a holistic approach to health or providing case management which improved several health and safety outcomes (Weber, 2019). Nurse-led interventions may be a crucial component of homeless patient health in hospitals.
The National Health Care for the Homeless Council has published recommendations for physicians providing care to patients who are homeless (Bonin E. et al., 2010). They several areas for physicians to consider when assessing and developing treatment plans (Bonin E. et al., 2010). These standards emphasize the use of integrated and flexible service delivery types as well as community outreach (Bonin E. et al., 2010). Patient safety in regards to the possible environmental dangers, abuse, or other patient risks that may need to be addressed in addition to the presenting concerns (Bonin E. et al., 2010).
Although not specifically assessed in patients who were homeless, hospital violence of patients to staff has been reported (Arnetz et al., 2015). Nurses, security, and nursing assistants were the most likely staff to report a violent incident with a patient (Arnetz et al., 2015). The times when violence was most likely to occur included during transfers, pain, using needles or restraints, and a patient wanting to leave (Arnetz et al., 2015). To ensure staff safety, it was recommended that a modified social-ecological model should be utilized to address safety concerns at the individual, relationship, work environment, and organization levels (Arnetz et al., 2015). The individual level (patient factors) included the patients’ feelings of pain and discomfort and cognitive impairment (Arnetz et al., 2015). Stressors like being moved or pricked by needles are the relationship level between patient and healthcare worker (Arnetz et al., 2015). The work environment may include the restraints used against patients, moving the patients, and similar situations (Arnetz et al., 2015). The organizational level is any hospital policies and systems which may influence the way patients and hospital staff interact with one another (Arnetz et al., 2015). The use of this modified social-ecological model may help practitioners identify areas where staff safety may be improved (Arnetz et al., 2015), and may be applicable to those serving patients who are homeless.
GUIDANCE FOR POLICIES AND INTERVENTIONS IN NON-U.S. HOSPITALS
There have been many interventions and policy changes internationally to improve the treatment of the homeless population. Based on research in Australia, it is recommended that physicians and other healthcare workers try to be as judgmental as possible in their interactions with patients who are homeless and keep consultations under 30 minutes with low health literacy to try to have the best outcomes (Davies & Wood, 2018). Six key best practices were identified to improve the health of the homeless population (Davies & Wood, 2018). First, treating finding housing as a means of healthcare and finding permanent housing solutions for patients is critical (Davies & Wood, 2018). Prioritizing the continuity of care despite the transient nature of the population may be accomplished with staff who have been linked with the patients previously (Davies & Wood, 2018). General practices which emphasize treating the homeless population are encouraged to help build relationships and provide more long-term solutions and support, even possibly connections for housing in the community (Davies & Wood, 2018). Hospital in-reach, also known as a specialized general practitioner in the hospital setting, can be an ideal way to link hospitalized patients with community resources and traditional general practitioners in the community (Davies & Wood, 2018). Individualized discharge planning and coordinated care are important, but it may be valuable to have a national-level policy to address the coordination of care to reduce readmission rates (Davies & Wood, 2018). Outreach by the general practitioner to homeless patients is necessary to ensure proper follow-up care is received (Davies & Wood, 2018). It may be beneficial to have drop-in clinics that do not require appointments or clinics within the shelters to reduce barriers to accessing care, though, these measures may not reach all, and street outreach may be valuable through mobile clinics or other means (Davies & Wood, 2018). The last best practice identified was the medical recovery center aimed to treat patients that need to be discharged from a hospital but are not healthy enough to return to the streets such as elective outpatient surgeries (Davies & Wood, 2018). These centers help reduce the number of readmissions and improve the health of patients who are homeless (Davies & Wood, 2018).
St. Vincent’s Hospital in Melbourne, Australia has comprehensive programs and policies to care for patients who are homeless (Wood et al., 2017). Four programs were highlighted as beneficial to improving the quality of life of homeless patients including the following: Assessment, Liaison, & Early Referral Team (ALERT); The Cottage; Prague House; and Clarendon Homeless Outreach Psychiatric Service (CHOPS)
(Wood et al., 2017). The ALERT program is targeted at patients in the emergency department to provide multidisciplinary treatment and coordinate discharge into a safe environment (Wood et al., 2017). CHOPS is a multidisciplinary team that conducts outreach in the community to treat those with mental illnesses (Wood et al., 2017). The Cottage is a small-scale healthcare treatment area designed to feel more home-like than a traditional hospital but with nursing and personal care workers (Wood et al., 2017). Similarly, The Prague House is an aged care home for older individuals with mental health issues that were previously homeless (Wood et al., 2017). These innovative approaches to treatment for homeless patients have been cost-effective measures that reduced hospitalizations and readmittance, and the value was recognized by both the patients and the healthcare workers (Wood et al., 2017).
Some national policies have been adopted to ensure the health and safety of homeless patients. The United Kingdom outlined hospital discharge recommendations (Homelessness and Health Information Sheet, 2005). These policies included patient coordinators, homelessness prevention coordinators, and housing services directives to reduce homelessness after discharge (Homelessness and Health Information Sheet, 2005). Despite these recommendations, an estimated 40% of hospitals were non-compliant in the four years after (Gallaher et al., 2020; Improving Hospital Admission and Discharge for People who are Homeless, 2012). As of 2013, one hospital policy did not include information regarding the discharge of homeless patients to a place of safety and that a social work referral was not appropriate as the homeless patients were not under their jurisdiction (Barrow & Medcalf, 2019). This lack of clear policy and disconnect in services likely had negative ramifications for the homeless population, thus they implemented a policy to include a hospital in-reach housing officer to help address the specific housing needs of patients who were homeless (Barrow & Medcalf, 2019). In the first year of the program, over 80% of homeless patients were referred to drug and alcohol services and were discharged into some form of housing (Barrow & Medcalf, 2019). Furthermore, staff attitudes towards the discharge of patients who were homeless improved, and staff were more likely to not discharge homeless patients until housing was secured and to refer to the in-reach housing officer (Barrow & Medcalf, 2019).
Another hospital in London began the “Homeless Health Initiative” to address shortcomings in the emergency department related to the homeless population (Gallaher et al., 2020). This initiative created a discharge checklist for staff and “Homeless Health Boxes” in the emergency department and formal and informal staff positions to focus on homeless health and not release patients to harmful environments (Gallaher et al., 2020). The interventions were considered cost-effective and provided valuable improvement to the treatment of homeless patients (Gallaher et al., 2020). Though the “Homeless Health Boxes” were a valuable tool in England, it lacked community outreach and training for non-medical staff (Gallaher et al., 2020). The “Homeless Health Initiative” may be especially helpful for hospitals with a large patient population that is homeless (Gallaher et al., 2020) but should prioritize additional training for non-medical staff within the hospital as well.
In Canada, a comparison was done between homeless men with mental illness who were treated with two types of shelter-based programs (Stergiopoulos et al., 2015). The first program was the integrated multidisciplinary collaborative care model which has a health team in the shelter on-site who work directly with shelter staff (Stergiopoulos et al., 2015). The second program was the shifted outpatient collaborative care model where an unrelated consultant visits and provides care at a shelter (Stergiopoulos et al., 2015). Overall, both programs provided valuable improvements in community functioning and did not significantly differ as well as a reduction in the emergency room/other acute care visits (Stergiopoulos et al., 2015).
A recent meta-analysis of interventions for discharging mental health patients included several focused on homeless populations and the most popular intervention noted was the Critical Time Intervention (CTI) (Tyler et al., 2019). The CTI is comprised of three phases in the time after a hospital discharge including the transition, the try-out, and the transfer of care phases (Tyler et al., 2019). The CTI was found to be successful in both reducing hospital readmissions as well as reducing homelessness of the patients (Tyler et al., 2019). The Transition Discharge Model (TDM) was a similar intervention which reduced helped encourage earlier discharges from the hospitals and reduce readmissions (Tyler et al., 2019). Contact-based interventions were helpful in maintaining adherence to medication but generally did not reduce readmittance (Tyler et al., 2019). Three types of role-based interventions were successful in improving at least one metric that was not readmission including the following newly implemented roles: community-based discharge team, community links team, and nursing discharge program (Tyler et al., 2019). Furthermore, other studies found success by assisting with securing housing or making rent payments, pharmacy interventions, and multi-level models were also evidenced in the review, though many did not have many studies to support the evidence (Tyler et al., 2019).
In Denmark, medical respite care was provided for 14 days for the homeless population after a short hospitalization (Pedersen et al., 2018). Medical respite after hospitalization provided patients with feelings of safety and security in addition to basic needs and social support (Pedersen et al., 2018). The respite care allowed for basic needs to be met and a stable place to rest which may help improve both mental and physical health outcomes (Pedersen et al., 2018).
An evaluation of dual-diagnosed homeless patients with a mental health disorder and a substance abuse disorder provided insight into effective treatment strategies (O’Campo et al., 2009). Specific considerations for interventions include patient collaboration for treatment decisions, multidisciplinary community treatments, both housing and other instrumental needs, and non-restrictive programs (O’Campo et al., 2009). This population may benefit from a long-term recovery program such as Sustainable Residence to reduce their danger to themselves and others (O’Campo et al., 2009; van Kranenburg et al., 2019). In the Netherlands, the Sustainable Residence program was designed to provide compulsory treatment for mental illness and substance abuse disorders (van Kranenburg et al., 2019). This multidisciplinary treatment approach was shown to improve functional improvements and reduced risk to self which allowed over 40% of patients to be discharged to a less restrictive setting (van Kranenburg et al., 2019). Despite improvements in a large percentage of the patients, there were some patients who required more restrictive treatment long-term which was largely determined by the danger to self and staff (van Kranenburg et al., 2019).
With regard to safety in emergency rooms and hospitals, a survey in Canada revealed that mental health nurses were twice as likely to have policies to physically intervene with patients than medical-surgical nurses (Havaei et al., 2019). Fixed alarms were present for most mental health nurses and were associated with how nurses perceived safety (Havaei et al., 2019). Other prevention strategies that were related to perceptions of safety included having enough trained personnel, feelings of support by employers for staff suggestions, and not having policies for nurses to physically intervene (Havaei et al., 2019). Though de-escalation training can be beneficial (Pich & Kable, 2014), training alone was not enough to influence nurses’ perceptions of safety (Havaei et al., 2019). Since perceptions of violence are often tied to the work environment rather than the patients themselves, it is critical hospital administrators ensure the setting is conducive to safety (Roche et al., 2010) and should include nurses in the conversation about workplace safety expectations (Havaei et al., 2019). Security measures such as faster security response times, zero-tolerance policies, and restricted access to safe rooms may also be appropriate to reduce violence (Pich & Kable, 2014).
SYNTHESIS OF THEMES
Homeless populations are generally not part of primary care physicians and thus require more acute care (Davies & Wood, 2018). Patients who were homeless were more likely to be readmitted after a short period of time (Racine et al., 2020). Differences in the diagnosis and treatment of diseases may be less proactive in the homeless population (Miyawaki et al., 2021), and can lead to delayed treatment (Festa et al., 2020). Negative perceptions and a lack of follow-up from healthcare providers may inhibit homeless health-seeking behaviors (Franco et al., 2021; Prado et al., 2021). Furthermore, there are often many challenging social issues that may negatively affect health (Moore et al., 2011) and may lead to visiting the emergency department for non-emergent needs as frequent flyers.
Many homeless individuals have at least one mental illness that may increase safety risks for patients and hospital staff (Fazel et al., 2008). Substance abuse and alcohol dependence were most prevalent among the homeless population (Fazel et al., 2008; Schreiter et al., 2017). veterans had a high incidence of opioid usage disorders and suicide attempts (Soncrant et al., 2021). Recent prior violence was very common among homeless patients with severe mental illness (Fond et al., 2019). Homeless patients were more likely to successfully complete suicide in in-patient treatment compared to those who committed suicide and were not homeless (Arnetz et al., 2015). These mental health and safety concerns may help inform programs and interventions which may be beneficial for homeless patients.
Policies and interventions that support connection from the hospital to the community upon discharge are integral in treating and discharging patients who are homeless. A variety of interventions have been successful in both the hospital and community settings (Tyler et al., 2019; Weber, 2019). There are many innovative approaches to improve health and safety among the homeless population.
RECOMMENDATIONS AND IMPLEMENTATION
Safety-net hospitals generally have a higher percentage of homeless patients than other hospitals, yet often do not have enough resources to adequately treat these patients (Figueroa et al., 2017). However, it is crucial that special care is taken to ensure the safety of homeless patients, and this can be a cost-effective way to improve health (Improving Hospital Admission and Discharge for People who are Homeless, 2012). Therefore, there are several recommendations for healthcare practices that serve the homeless population to promote health (see tables below).
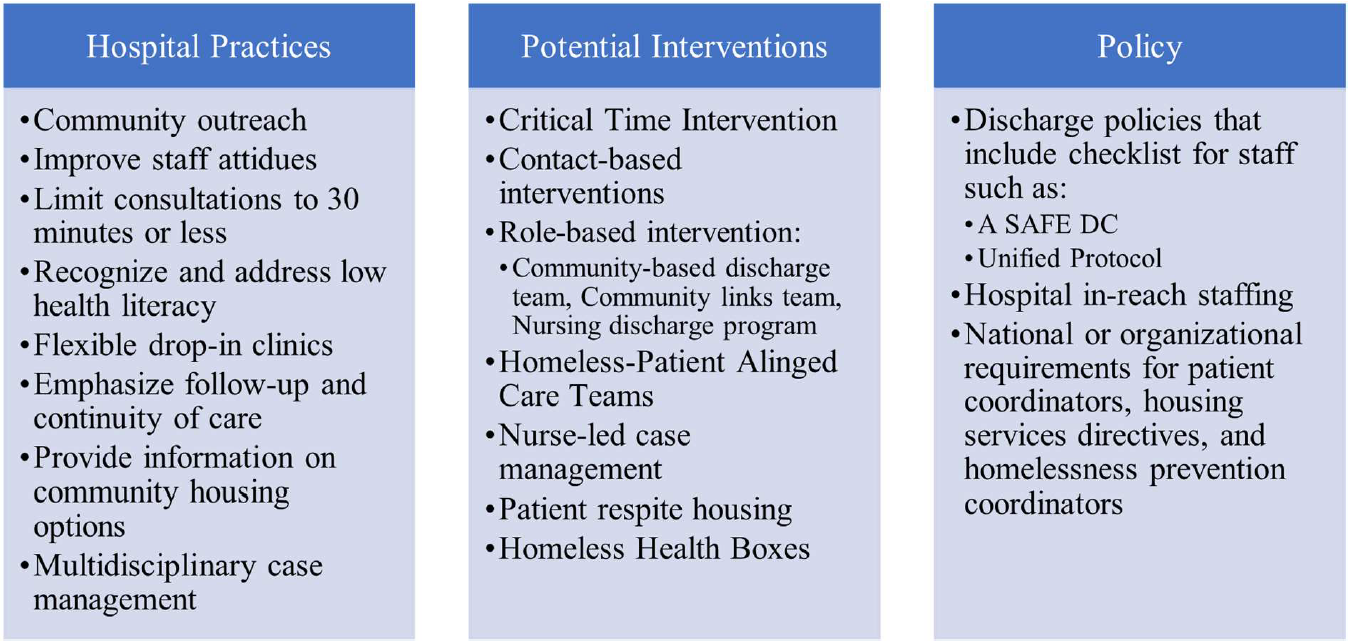
Before any intervention or policy can be implemented, the attitudes of staff toward homeless patients should be addressed. People who are homeless reported that their providers’ attitude toward them negatively affected their care (Franco et al., 2021). Homeless patients will likely feel judged more than other patients, thus it is important for practitioners to consider how they interact with these patients (Davies & Wood, 2018). Developing relationships with patients when possible is key to helping improve follow-up (Davies & Wood, 2018).
Hospital readmissions were lower when homeless patients had a primary care practitioner (Racine et al., 2020). Homeless-Patient Aligned Care Teams (Gabrielian et al., 2021), short-term respite housing options (Wood et al., 2017), and nurse-led interventions (Weber, 2019) were valuable tools for measurably improving patient health and satisfaction. Multidisciplinary case management was also helpful to reduce frequent flyers in hospital emergency rooms (Phillips et al., 2006). Consider implementing collaborative care for treatment decisions, especially among patients who also have a mental illness (O’Campo et al., 2009). Also, opioid prescribers, especially those prescribing to homeless veterans, should seek to provide Naloxone prescription and medicine for addiction treatment (Midboe et al., 2019) to hopefully reduce suicide and overdose risk (Midboe et al., 2019; Soncrant et al., 2021).
Community outreach and hospital in-reach are also essential aspects of caring for the homeless population. Outreach to the community with flexible drop-in clinics (Bonin E. et al., 2010; Davies & Wood, 2018) and multidisciplinary outreach to people living on the streets with mental illnesses should be considered (Wood et al., 2017). Hospital in-reach could involve a general practitioner to link homeless patients to other traditional practitioners or community resources (Davies & Wood, 2018) or a housing officer to help connect homeless patients with housing opportunities or further treatment opportunities (Barrow & Medcalf, 2019). Lowering the barrier to access care in the community and after discharge is a valuable aspect of healthcare.
Comprehensive discharge procedures/checklists may help healthcare workers provide consistent quality care for homeless patients. “A SAFE-DC” (Best & Young, 2009), the Unified Protocol (Sauer-Zavala et al., 2019), “Homeless Health Initiative” (Gallaher et al., 2020), and the ALERT program (Wood et al., 2017) all had discharge policies specifically designed to improve patient safety upon discharge. Implementing a discharge checklist may encourage staff to better refer patients who are homeless to the appropriate resources in the community.
Flexible housing options are also valuable. Mental health residences for compulsory treatment like the Sustainable Residence program can help improve patient functioning and safety (van Kranenburg et al., 2019). Respite care after hospitalization can improve social support and health outcomes after a hospitalization (Pedersen et al., 2018). A more home-like atmosphere for recovery after hospitalization for those who are not able to return to their previous environment like the Cottage (Wood et al., 2017) may be added to healthcare centers serving homeless populations. Housing homeless patients, even short term, can provide valuable time to heal and recover for a safer discharge. Overall, there was a lack of information available regarding safety and security practices for inpatient homeless individuals, yet hospital violence is present in many hospitals, especially against nurses (Arnetz et al., 2015). Therefore, a modified social-ecological model featuring individual, relationship, work environment, and organization levels (Arnetz et al., 2015) can help identify areas of safety concern for patients (Arnetz et al., 2015). This framework can be considered within more general patient safety guidelines for hospital settings such as those published by the International Association for Healthcare Security and Safety (IAHSS) (International Association for Healthcare Security and Safety (IAHSS), 2020, 2021).
Strengths and Limitations
The present review highlights many valuable tools and resources that can be implemented. Understanding the patient risks of the homeless population can provide valuable insight into issues that may arise. There were a variety of interventions that target many aspects of patient care that are more common among patients who are homeless. Many of these practices can be cost-effective measures to help improve patient health and well-being. Incorporating interventions, especially multilevel interventions, may have a dramatic impact on homeless patients.
There are some limitations to the present study and the information available on the topic. First, there was an overall lack of literature available on violence in emergency room and hospital settings for homeless patients. Additionally, not all studies used the same metrics for success which can limit overall comparison. While there were a variety of studies from around the world, specific conditions within each country may limit generalizability to other parts of the world. Also, few national policies existed to outline homeless patient discharge procedures and were not always adhered to by individual hospitals (Gallaher et al., 2020).
Future Considerations
Matriculating physician’s assistants were evaluated to measure their attitude towards and knowledge about people who were homeless prior to their school career (Feldman et al., 2020). Though most had positive attitudes, the results show students were excited to learn more about how to treat the homeless population and understand specific burdens known to be associated with this population (Feldman et al., 2020). Thus, the school curriculum may be improved by including training on treating the homeless with dignity and understanding the mental health and other difficulties faced by this specific population (Feldman et al., 2020). The lack of evidence of violence including homeless patients in the emergency room highlights an area of research that should be considered. Finally, more national and hospital policies should consider specific recommendations for homeless patients within their care.
CONCLUSION
The homeless population is a vulnerable group of people without typical access to care and social support. Therefore, healthcare providers provide critical support to the homeless patients they treat. Health, overall safety, and general patient satisfaction can be improved with a variety of interventions. Hospitals and other healthcare providers should consider ways they could improve their attitude and support of patients who are homeless through in-hospital measures or community outreach.
AUTHOR
Christen Dunn holds a Master of Public Health degree and is pursuing a Ph.D. in Health Services Research at Old Dominion University in Norfolk, Va. Ms. Dunn’s current research interests include sleep and mental health related outcomes in a variety of populations.
REFERENCES
Arnetz, J. E., Hamblin, L., Essenmacher, L., Upfal, M. J., Ager, J., & Luborsky, M. (2015). Understanding patient-to-worker violence in hospitals: a qualitative
analysis of documented incident reports. Journal of advanced nursing, 71(2), 338-348. https://doi.org/10.1111/jan.12494
Barrow, V., & Medcalf, P. (2019). The introduction of a homeless healthcare team in hospital improves staff knowledge and attitudes towards homeless patients. Clin Med (Lond), 19(4), 294-298. https://doi.org/10.7861/clinmedicine.19-4-294
Best, J. A., & Young, A. (2009). A SAFE DC: a conceptual framework for care of the homeless inpatient. J Hosp Med, 4(6), 375-381. https://doi.org/10.1002/jhm.568
Bonin E., Brehove T, Carlson C, Downing M, Hoeft J, Kalinowski A, Solomon-Bame J, & P., P. (2010). Adapting Your Practice: General Recommendations for the Care of Homeless Patients. Health Care for the Homeless Clincian’s Network, National Health Care for the Homeless Cousil, Inc.
Cimino, T., Steinman, M. A., Mitchell, S. L., Miao, Y., Bharel, M., Barnhart, C. E., & Brown, R. T. (2015). The Course of Functional Impairment in Older Homeless Adults: Disabled on the Street. JAMA Intern Med, 175(7), 1237-1239. https://doi.org/10.1001/jamainternmed.2015.1562
Cox, K. B., Malte, C. A., & Saxon, A. J. (2017). Characteristics and service utilization of homeless veterans entering VA substance use treatment. Psychological Services, 14(2), 208-213. https://doi.org/10.1037/ser0000133
Culatto, P., Bojanić, L., Appleby, L., & Turnbull, P. (2021). Suicide by homeless patients in England and Wales: national clinical survey. BJPsych Open, 7(2), e65. https://doi.org/10.1192/bjo.2021.2
Dale E. McNiel, Ph.D. , and, & Renée L. Binder, M.D. (2005). Psychiatric Emergency Service Use and Homelessness, Mental Disorder, and Violence. Psychiatric Services, 56(6), 699-704. https://doi.org/10.1176/appi.ps.56.6.699
Davies, A., & Wood, L. J. (2018). Homeless health care: meeting the challenges of providing primary care. Med J Aust, 209(5), 230-234. https://doi.org/10.5694/mja17.01264
Dell, K. C., Staph, J., & Hillary, F. G. (2021). Traumatic brain injury in the homeless: health, injury mechanisms, and hospital course. Brain Injury, 35(10), 1192-1200. https://doi.org/10.1080/02699052.2021.1958009
Fazel, S., Khosla, V., Doll, H., & Geddes, J. (2008). The prevalence of mental disorders among the homeless in western countries: systematic review and meta regression analysis. PLoS Med, 5(12), e225. https://doi.org/10.1371/journal.pmed.0050225
Feldman, C. T., Stevens, G. D., Lowe, E., & Lie, D. A. (2020). Inclusion of the homeless in health equity curricula: a needs assessment study. Med Educ Online, 25(1), 1777061. https://doi.org/10.1080/10872981.2020.1777061
Festa, K., Hirsch, A. E., Cassidy, M. R., Oshry, L., Quinn, K., Sullivan, M. M., & Ko, N. Y. (2020). Breast Cancer Treatment Delays at an Urban Safety Net Hospital Among Women Experiencing Homelessness. Journal of Community Health, 45(3), 452-457. https://doi.org/https://doi.org/10.1007/s10900-019-00759-x
Figueroa, J. F., Joynt, K. E., Zhou, X., Orav, E. J., & Jha, A. K. (2017). Safety-net Hospitals Face More Barriers Yet Use Fewer Strategies to Reduce Readmissions. Med Care, 55(3), 229-235. https://doi.org/10.1097/mlr.0000000000000687
Fond, G., Boyer, L., Boucekine, M., Girard, V., Loubière, S., Lenoir, C., Auquier, P., & Tinland, A. (2019). Illness and drug modifiable factors associated with violent behavior in homeless people with severe mental illness: results from the French Housing First (FHF) program. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 90, 92-96. https://doi.org/https://doi.org/10.1016/j.pnpbp.2018.11.006
Franco, A., Meldrum, J., & Ngaruiya, C. (2021). Identifying homeless population needs in the Emergency Department using Community-Based Participatory Research. BMC Health Serv Res, 21(1), 428. https://doi.org/10.1186/s12913-021-06426-z
Fulde, G. W. O., & Duffy, M. (2006). Emergency department frequent flyers: unnecessary load or a lifeline? Medical journal of Australia, 184(12), 595-595. https://doi.org/10.5694/j.1326-5377.2006.tb00407.x
Gabrielian, S., Jones, A. L., Hoge, A. E., deRussy, A. J., Kim, Y.-i., Montgomery, A. E., Blosnich, J. R., Gordon, A. J., Gelberg, L., Austin, E. L., Pollio, D., Holmes, S. K., Varley, A. L., & Kertesz, S. G. (2021). Enhancing Primary Care Experiences for Homeless Patients with Serious Mental Illness: Results from a National Survey. Journal of Primary Care & Community Health, 12, 2150132721993654. https://doi.org/10.1177/2150132721993654
Gallaher, C., Herrmann, S., Hunter, L., & Wilkins, A. (2020). The St Thomas’ Hospital Emergency Department Homeless Health Initiative: improving the quality, safety and equity of healthcare provided for homeless patients attending the ED. BMJ Open Qual, 9(1). https://doi.org/10.1136/bmjoq-2019-000820
Gordon, J. A., Chudnofsky, C. R., & Hayward, R. A. (2001). Where health and welfare meet: social deprivation among patients in the emergency department. J Urban Health, 78(1), 104-111. https://doi.org/10.1093/jurban/78.1.104
Gummerson, S., Smith, M., & Warren, O. (2022). Effect of an Emergency Department Closure on Homeless Patients and Adjacent Hospitals. West J Emerg Med, 23(3), 368-374. https://doi.org/10.5811/westjem.2021.12.53918
Han, B., & Wells, B. L. (2003). Inappropriate Emergency Department Visits and Use of the Health Care for the Homeless Program Services by Homeless Adults in the Northeastern United States. Journal of Public Health Management and Practice,
9(6). https://journals.lww.com/jphmp/Fulltext/2003/11000/Inappropriate_Emergency_D epartment_Visits_and_Use.14.aspx
Hanssmann, C., Shim, J. K., Yen, I. H., Fleming, M. D., Van Natta, M., Thompson-Lastad, A., Rasidjan, M. P., & Burke, N. J. (2022). “Housing Is Health Care”: Treating Homelessness in Safety-net Hospitals. Med Anthropol Q, 36(1), 44-63. https://doi.org/10.1111/maq.12665
Havaei, F., MacPhee, M., & Lee, S. E. (2019). The effect of violence prevention strategies on perceptions of workplace safety: A study of medical‐surgical and mental health nurses. Journal of advanced nursing, 75(8), 1657-1666. https://doi.org/10.1111/jan.13950
Henry, M., Watt, R., Rosenthal, L., & Shivji, A. (2018). The 2018 annual homeless assessment report (AHAR) to Congress, part 1: Point-in-Time estimates of homelessness. The US Department of Housing and Urban Development.
Homelessness and Health Information Sheet. (2005). United Kingdom Retrieved from https://nhchc.org/wp-content/uploads/2019/08/137857.pdf
Hwang, S. W., & Burns, T. (2014). Health interventions for people who are homeless. The Lancet, 384(9953), 1541-1547. https://doi.org/https://doi.org/10.1016/S0140-6736(14)61133-8
Ijaz, S., Jackson, J., Thorley, H., Porter, K., Fleming, C., Richards, A., Bonner, A., & Savović, J. (2017). Nutritional deficiencies in homeless persons with problematic drinking: a systematic review. Int J Equity Health, 16(1), 71. https://doi.org/10.1186/s12939-017-0564-4
Improving Hospital Admission and Discharge for People who are Homeless. (2012). https://www.housinglin.org.uk/_assets/Resources/Housing/OtherOrganisation/Improving_hospital_admission_and_discharge_for_people_who_are_homeless.PDF
International Association for Healthcare Security and Safety (IAHSS). (2020). Security Design Guidelines for Healthcare Facilities. In (3rd ed.). Chicago, IL 60631: International Association for Healthcare Security and Safety (IAHSS).
International Association for Healthcare Security and Safety (IAHSS). (2021). HEALTHCARE SECURITY INDUSTRY GUIDELINES. In (13th ed.). Chicago, IL 60631: International Association for Healthcare Security and Safety (IAHSS).
Jackson, T. S., Moran, T. P., Lin, J., Ackerman, J., & Salhi, B. A. (2019). Homelessness Among Patients in a Southeastern Safety Net Emergency Department. Southern medical journal (Birmingham, Ala.), 112(9), 476-482. https://doi.org/10.14423/SMJ.0000000000001016
Kryda, A. D., & Compton, M. T. (2008). Mistrust of Outreach Workers and Lack of Confidence in Available Services Among Individuals who are Chronically Street Homeless. Community Mental Health Journal, 45(2), 144. https://doi.org/10.1007/s10597-008-9163-6
Lam, C. N., Arora, S., & Menchine, M. (2016). Increased 30-Day Emergency Department Revisits Among Homeless Patients with Mental Health Conditions. The western journal of emergency medicine, 17(5), 607-612. https://doi.org/10.5811/westjem.2016.6.30690
Lin, W.-C., Bharel, M., Zhang, J., O’Connell, E., & Clark, R. E. (2015). Frequent Emergency Department Visits and Hospitalizations Among Homeless People With Medicaid: Implications for Medicaid Expansion. American Journal of Public Health, 105 Suppl 5, S716-S722. https://doi.org/https://doi.org/10.2105/AJPH.2015.302693
Malone, R. E. (1998). Whither the almshouse? Overutilization and the role of the emergency department. Journal of health politics, policy and law, 23(5), 795-832. http://proxy.lib.odu.edu/login?url=https://www.proquest.com/scholarlyjournals/whither-almshouse-overutilization-roleemergency/docview/70030257/se-2?accountid=12967
McMillan, T. M., Laurie, M., Oddy, M., Menzies, M., Stewart, E., & Wainman-Lefley, J. (2015). Head injury and mortality in the homeless. J Neurotrauma, 32(2), 116-119. https://doi.org/10.1089/neu.2014.3387
Meinbresse, M., Brinkley-Rubinstein, L., Grassette, A., Benson, J., Hall, C., Hamilton, R., Malott, M., & Jenkins, D. Exploring the Experiences of Violence Among Individuals Who Are Homeless Using a Consumer-Led Approach. Violence Vict(1), 122-136. https://doi.org/10.1891/0886-6708.VV-D-12-00069
Michelen, W., Martinez, J., Lee, A., & Wheeler, D. P. (2006). Reducing Frequent Flyer Emergency Department Visits. Journal of Health Care for the Poor and Underserved, 17(1), 59-69.
Midboe, A. M., Byrne, T., Smelson, D., Jasuja, G., McInnes, K., & Troszak, L. K. (2019). The Opioid Epidemic In Veterans Who Were Homeless Or Unstably Housed. Health Affairs, 38(8), 1289-1297. https://doi.org/10.1377/hlthaff.2019.00281
Miyawaki, A., Khullar, D., & Tsugawa, Y. (2021). Processes of care and outcomes for homeless patients hospitalised for cardiovascular conditions at safety-net versus non-safety-net hospitals: cross-sectional study. BMJ Open, 11(4), e046959. https://doi.org/10.1136/bmjopen-2020-046959
Moore, G., Manias, E., & Gerdtz, M. F. (2011). Complex health service needs for people who are homeless. Australian Health Review, 35(4), 480-485.
O’Campo, P., Kirst, M., Schaefer-McDaniel, N., Firestone, M., Scott, A., & McShane, K. (2009). Community-based services for homeless adults experiencing concurrent mental health and substance use disorders: a realist approach to synthesizing evidence. J Urban Health, 86(6), 965-989. https://doi.org/10.1007/s11524-009-9392-1
Omerov, P., Craftman, Å. G., Mattsson, E., & Klarare, A. (2020). Homeless persons’ experiences of health- and social care: A systematic integrative review. Health & Social Care in the Community, 28(1), 1-11. https://doi.org/https://doi.org/10.1111/hsc.12857
Patten, S. B. (2017). Homelessness and Mental Health. Canadian journal of psychiatry. Revue canadienne de psychiatrie, 62(7), 440-441. https://doi.org/10.1177/0706743717711423
Pedersen, M., Bring, C., Brünés, N., Andersen, O., Petersen, J., & Jarden, M. (2018). Homeless people’s experiences of medical respite care following acute hospitalisation in Denmark. Health & Social Care in the Community, 26(4), 538- 46. https://doi.org/https://doi.org/10.1111/hsc.12550
Phillips, G. A., Brophy, D. S., Weiland, T. J., Chenhall, A. J., & Dent, A. W. (2006). The effect of multidisciplinary case management on selected outcomes for frequent attenders at an emergency department. Medical journal of Australia, 184(12), 602-606. https://doi.org/10.5694/j.1326-5377.2006.tb00412.x
Pich, J., & Kable, A. (2014). Patient-related violence against nursing staff working in emergency departments: a systematic review. JBI Evidence Synthesis, 12(9). https://journals.lww.com/jbisrir/Fulltext/2014/12090/Patient_related_violence_against_nursing_staff.19.aspx
Prado, M., Gonçalves, M., Silva, S. S. D., Oliveira, P. S., Santos, K. D. S., & Fortuna, C. M. (2021). Homeless people: health aspects and experiences with health services. Rev Bras Enferm, 74(1), e20190200. https://doi.org/10.1590/0034-7167-2019-0200
Racine, M. W., Munson, D., Gaeta, J. M., & Baggett, T. P. (2020). Thirty-Day Hospital Readmission Among Homeless Individuals With Medicaid in Massachusetts. Med Care, 58(1), 27-32. https://doi.org/10.1097/mlr.0000000000001234
Roche, M., Diers, D., Duffield, C., & Catling-Paull, C. (2010). Violence toward nurses, the work environment, and patient outcomes. J Nurs Scholarsh, 42(1), 13-22. https://doi.org/10.1111/j.1547-5069.2009.01321.x
Rodriguez, R. M., Fortman, J., Chee, C., Ng, V., & Poon, D. (2009). Food, Shelter and Safety Needs Motivating Homeless Persons’ Visits to an Urban Emergency Department. Annals of emergency medicine, 53(5), 598-602.e591. https://doi.org/https://doi.org/10.1016/j.annemergmed.2008.07.046
Ruger, J. P., Richter, C. J., Spitznagel, E. L., & Lewis, L. M. (2004). Analysis of costs, length of stay, and utilization of emergency department services by frequent users: implications for health policy. Acad Emerg Med, 11(12), 1311-1317. https://doi.org/10.1197/j.aem.2004.07.008
Sauer-Zavala, S., Ametaj, A. A., Wilner, J. G., Bentley, K. H., Marquez, S., Patrick, K. A., Starks, B., Shtasel, D., & Marques, L. (2019). Evaluating transdiagnostic, evidence-based mental health care in a safety-net setting serving homeless individuals. Psychotherapy (Chic), 56(1), 100-114. https://doi.org/10.1037/pst0000187
Schinka, J. A., Leventhal, K. C., Lapcevic, W. A., & Casey, R. (2018). Mortality and Cause of Death in Younger Homeless Veterans. Public health reports (Washington, D.C. : 1974), 133(2), 177-181. https://doi.org/10.1177/0033354918755709
Schneider, M., Brisson, D., & Burnes, D. (2016). Do We Really Know how Many Are Homeless?: An Analysis of the Point-In-Time Homelessness Count. Families in Society, 97(4), 321-329. https://doi.org/10.1606/1044-3894.2016.97.39
Schreiter, S., Bermpohl, F., Krausz, M., Leucht, S., Rössler, W., Schouler-Ocak, M., & Gutwinski, S. (2017). The Prevalence of Mental Illness in Homeless People in Germany. Dtsch Arztebl Int, 114(40), 665-672. https://doi.org/10.3238/arztebl.2017.0665
Soncrant, C., Mills, P. D., Pendley Louis, R. P., & Gunnar, W. (2021). Review of Reported Adverse Events Occurring Among the Homeless Veteran Population in the Veterans Health Administration. J Patient Saf, 17(8), e821-e828.
https://doi.org/10.1097/pts.0000000000000884
Stergiopoulos, V., Schuler, A., Nisenbaum, R., deRuiter, W., Guimond, T., Wasylenki, D., Hoch, J. S., Hwang, S. W., Rouleau, K., & Dewa, C. (2015). The effectiveness of an integrated collaborative care model vs. a shifted outpatient collaborative care model on community functioning, residential stability, and health service use among homeless adults with mental illness: a quasiexperimental study. BMC Health Serv Res, 15(1), 348. https://doi.org/10.1186/s12913-015-1014-x
Tornero Patricio, S., Fernández Ajuria, A., & Charris Castro, L. (2016). Characteristics of Hospitalizations of Homeless Persons in Seville, Spain. Rev Esp Salud Publica, 90, E12. (Características de los ingresos hospitalarios de las personas sin hogar en Sevilla.)
Tyler, N., Wright, N., & Waring, J. (2019). Interventions to improve discharge from acute adult mental health inpatient care to the community: systematic review and narrative synthesis. BMC Health Serv Res, 19(1), 883. https://doi.org/10.1186/s12913-019-4658-0
van Dongen, S. I., Klop, H. T., Onwuteaka-Philipsen, B. D., de Veer, A. J. E., Slockers, M. T., van Laere, I. R., van der Heide, A., & Rietjens, J. A. C. (2020). End-of-life care for homeless people in shelter-based nursing care settings: A retrospective record study. Palliative Medicine, 34(10), 1374-1384. https://doi.org/10.1177/0269216320940559
van Kranenburg, G. D., van den Brink, R. H. S., Mulder, W. G., Diekman, W. J., Pijnenborg, G. H. M., & Mulder, C. L. (2019). Clinical effects and treatment outcomes of long-term compulsory in-patient treatment of treatment-resistant patients with severe mental illness and substance-use disorder. BMC Psychiatry, 19(1), 270. https://doi.org/10.1186/s12888-019-2254-9
Vellozzi-Averhoff, C., Thompson, W. W., Vellozzi, C., Okosun, I., Kinlaw, K., & Bussey-Jones, J. (2021). Disparities in communication among the inpatient homeless population at a safety-net hospital. J Natl Med Assoc, 113(4), 440-448. https://doi.org/10.1016/j.jnma.2021.02.009
Vohra, N., Paudyal, V., & Price, M. J. (2022). Homelessness and the use of Emergency Department as a source of healthcare: a systematic review. International Journal of Emergency Medicine, 15(1), 32. https://doi.org/10.1186/s12245-022-00435-3 Wadhera, R. K., Khatana, S. A. M., Choi, E., Jiang, G., Shen, C., Yeh, R. W., & Joynt Maddox, K. E. (2020). Disparities in Care and Mortality Among Homeless Adults Hospitalized for Cardiovascular Conditions. JAMA Intern Med, 180(3), 357-366. https://doi.org/10.1001/jamainternmed.2019.6010
Weber, J. J. (2019). A systematic review of nurse‐led interventions with populations experiencing homelessness. Public health nursing (Boston, Mass.), 36(1), 96-106. https://doi.org/10.1111/phn.12552
Wood, L., Vallesi, S., Martin, K., Lester, L., Zaretzky, K., Flatau, P., & Gazey, A. (2017). St Vincent’s Hospital Melbourne Homelessness Programs Evaluation Report. An evaluation of ALERT, CHOPS, The Cottage and Prague House. https://doi.org/10.13140/RG.2.2.34614.60480
Wright, N. M., Campbell, T. L., & Tompkins, C. N. (2002). Comparison of conventional and accelerated hepatitis B immunisation schedules for homeless drug users. Commun Dis Public Health, 5(4), 324-326.
Xiang, J., Kaminga, A. C., Wu, X. Y., Lai, Z., Yang, J., Lian, Y., Wang, X., Wen, S. W., Liu, A., & Dai, W. (2021). Lifetime prevalence of suicidal attempt among homeless individuals in North America: a meta-analysis. J Affect Disord, 287, 341-349. https://doi.org/10.1016/j.jad.2021.03.052
Download PDF copy of the document
