SYNTHESIS OF THEMES
Based on the literature and guidelines available regarding self-harm and suicide, a few key themes have emerged. First, more guidance and research has been provided for inpatient suicide prevention than self-harm prevention specifically. Nonetheless, these two topics are closely related and can have similar prevention strategies (Hawton et al., 2015). Suicide and self-harm attempts are usually the result of multiple stressors and other factors (Betz et al., 2016; de Beurs et al., 2018; Hawton et al., 2015; Navin et al., 2019; Townsend et al., 2016).
Similarly, self-harm and suicide prevention efforts are multifaceted and require coordination and training among hospital staff. Staff need training on how to properly interact with patients who are at risk and need increased confidence in their knowledge and ability to carry out necessary actions (Navin et al., 2019). Objects in the environment are a commonly used by patients to attempt suicide and self-harm in inpatient settings, so it is important for private areas and specific items to be monitored when a patient is at higher risk for suicide or self-harm (Mills et al., 2013; Mills et al., 2010; Navin et al., 2019). Multidisciplinary teams can address multiple dimensions of patient health and provide treatment that improves physical and mental health (Grant & Lusk, 2015).
Screening of patients who may have suicide ideation is an important step to adequately measure risk and allow for the best care plan possible (de Beurs et al., 2018; National Institute for Health and Care Excellence, 2013; The Joint Commission, 2020). Emergency rooms can screen patients as well, ensuring individuals are cared for prior to discharge (Olfson et al., 2012). Having a better understanding of a patient’s motives and history will allow for better care and a more effective plan of action for patients (de Beurs et al., 2018).
Another major theme emerged that limits the ability of researchers. A lack of consistent reporting and estimates of self-harm and suicide in inpatient settings can inhibit the ability to accurately track and measure the success of interventions. Although it is believed inpatient suicide has decreased recently in the United States (Matthay et al., 2018), there has been inconsistent reporting in different States and countries, making it difficult to estimate the true frequency (Reuter Morthorst et al., 2016; Walsh et al., 2015; Williams et al., 2018). More accurate reporting and surveillance of suicide and self-harm rates among individuals staying in a hospital will help provide better feedback on the efficacy of policies and practices implemented by the hospital to reduce risk.
Finally, policy plays a vital role in reducing inpatient suicide and self-harm. As part of the recognition of suicide as a global issue by the WHO, it was recommended that countries develop a plan to address suicide attempts and mitigate risk among their citizens (World Health Organization, 2014). Having policies in place such as the National Institute for Health and Care Excellence and The Joint Commission’s National Patient Safety Goals, promotes standardization of patient care (National Institute for Health and Care Excellence, 2013, 2019; The Joint Commission, 2020). Governments should seek to establish policies to help support hospital staff and protect patients experiencing self-harm or suicide ideation.
DISCUSSION
Suicide and patient self-harm is an area of patient safety that has been addressed in a variety of ways including hospital practices, environmental modification, staff education, and more. In the United States, The Joint Commission did not provide separate suicide and self-harm prevention. Reducing self-harm incidents was only addressed as a way to prevent eventual suicide (The Joint Commission, 2020). Similarly, Australia also included self-harm and suicide in the same action steps (Australian Commission on Safety and Quality in Health Care, 2017), but did not offer much guidance into how this should be carried out properly in a hospital. Meanwhile, the National Institute for Health and Care Excellence in the United Kingdom addressed both suicide and self-harm prevention at length and provides more practical applications of the guidance (National Institute for Health and Care Excellence, 2013, 2019). Hospitals and healthcare systems should aim to have more established and practical guidelines to ensure the appropriate standard of care is received.
Environment modification is included in the self-harm and suicide guidelines provided by The Joint Commission and the National Institute for Health and Care Excellence (National Institute for Health and Care Excellence, 2013, 2019; The Joint Commission, 2020). After the implementation of the Mental Health Environment of Care Checklist by the Department of Veterans Affairs in the United States, the agency was able to significantly reduce the number of inpatient suicides conducted at their hospitals. The extensive research aimed at understanding suicide in veteran inpatient populations and the sustained reduction in suicide rates among inpatients in veterans’ hospitals may provide useful guidance for other facilities.
Suicide attempts are more likely to occur in psychiatric hospitals and in private areas of a patient’s room (Williams et al., 2018). This aligns with findings in the creation and development of the Veterans Affairs Checklist (Mills et al., 2013; Mills et al., 2010), identifies those areas as being of utmost importance during observation and safety checks. Staff awareness of items and areas that can be utilized for self-harm or suicide is critical for all hospital staff to help mitigate risk. Patients may require more supervision in specific areas of higher risk (Navin et al., 2019).
While staff training is an important aspect for suicide prevention, many States do not require suicide prevention training (Graves et al., 2018). Furthermore, most of the suicide prevention trainings available are gatekeeper training not specific to the hospital staff (Litteken & Sale, 2018; Sanne et al., 2018). Short suicide prevention trainings have been shown to improve staff knowledge and capability (Berlim et al., 2007), but more can be done. Specific, comprehensive, and interdisciplinary trainings for hospital staff should be developed and required to better equip all staff to handle patients with suicidal ideation.
Despite these efforts to reduce the number of inpatient suicides, there does not seem to be a clear downward trend in inpatient suicides and self-harm incidents (Williams et al., 2018). However, as previously mentioned, without concrete data, it is challenging to accurately measure the impact these guidelines and practices are having on the issue.
RECOMMENDATIONS
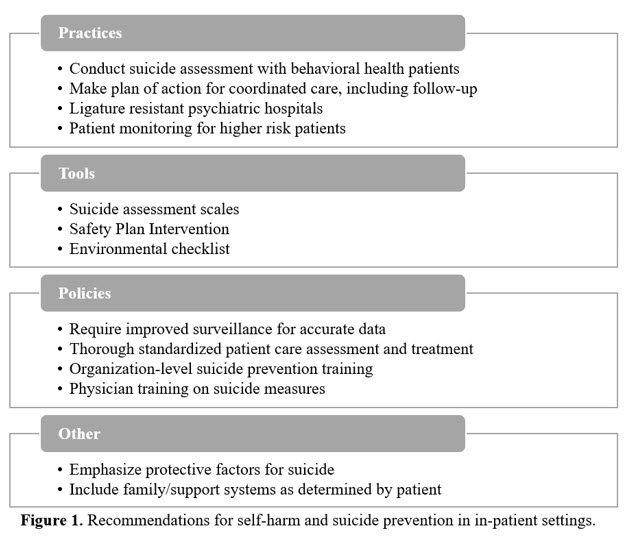
To mitigate suicide and self-harm risk in inpatient settings, there are several practices, tools, policies, and other interventions that can be utilized. Hospitals should seek to implement best practices when possible to reduce risk. These recommendations are a combination of practices and guidelines from around the world and are crucial to reducing the self-harm and suicide-related deaths in hospital settings (see Figure 1).
Practices
Every behavioral health patient should be assessed for current suicide and self-harm risk (de Beurs et al., 2018; Koweszko et al., 2016; National Institute for Health and Care Excellence, 2013, 2019; The Joint Commission, 2020). Risk assessment should include both clinical and psychological components to accurately determine patient risk of suicide or self-harm (Grant & Lusk, 2015; Wortzel et al., 2013). A determination of this risk can be utilized to develop a plan of action for the duration of the hospital stay and may include psychotherapy, medicine, or other forms of therapy to reduce suicide risk (Navin et al., 2019). The Safety-Plan Intervention methods may also be incorporated into the action plan to provide patients with coping strategies to prevent suicidal behavior (Stanley & Brown, 2012). Patient rooms should be ligature-resistant and monitored for other potentially hazardous areas and items that may be used for self-harm (The Joint Commission, 2020). Patients with higher risk may require more frequent observation or even constant observation (Navin et al., 2019; Russ, 2016). Psychosocial therapy should be considered for patients who have previously self-harmed (Birkbak et al., 2016).
Tools
There are a few tools that may mitigate self-harm and suicide risk. First, a self-harm or suicide risk assessment can be used to evaluate patients on intake and reevaluate over time (de Beurs et al., 2018; Koweszko et al., 2016; National Institute for Health and Care Excellence, 2013, 2019; The Joint Commission, 2020) such as the Verbal Suicide Scale (Koweszko et al., 2016), the Columbia Suicide Severity Scale (Posner et al., 2011), the Beck Scale for Suicide Ideation (Beck, Steer, & Ranieri, 1988), or other self-reported suicide measures (Grant & Lusk, 2015). Emergency departments may also benefit from these assessments, which can prevent them from prematurely discharging patients who may still benefit from care (Olfson et al., 2012). Additionally, an environmental checklist such as the Mental Health Environment of Care Checklist may help identify areas and objects that are most likely to be utilized for suicide or self-harm attempts (Mills et al., 2013; Mills et al., 2010). The Safety-Planning Intervention may be utilized by physicians and other hospital staff to emphasize strategies the patient may use to withstand suicidal urges based on resources available during their hospital stay (Stanley & Brown, 2012).